04 Sep Step 1 How to manage the symptoms of Dry Eyes
Here we share the most recent comprehensive research on dry eye disease and how to potentially self manage.
Over a 2.5 year period, involving 150 clinicians and research experts from around the world, a global consensus on the treatment and management of dry eye disease was decided upon and compiled in a DEWS II report.
The severity of the symptoms varies between sufferers but the numbers are growing rapidly with an estimated 344 million people worldwide affected to some degree with dry eyes. As we adapt and come out of the latest pandemic, the restrictions associated with it, working from home, etc it is predicted that this figure is only going to rise. Smart classrooms and classes online have now turned children and young adults into potential sufferers. As we know, children pre-COVID utilized digital devices mainly for social and leisure purposes, now with education going more and more online, their usage has multiplied.
The outcome of this report is a 4-step plan to diagnose, manage, and treat all levels of dry eye disease.
In this article, I aim to cover the advice given in Step 1 (which is ground zero) and what we generally ask our patients to revert to when they initially attend our dry eye clinics. Our experience is that patients, in their desperation to self-manage the symptoms of dry eyes, jump from product to product with little strategy or ultimate effectiveness.
A fundamental understanding that dry eyes need to be managed on a long-term basis and patients need to realize this, in many cases, an ultimate cure is not available. Patients go through cycles of dry eye issues and management needs to be stepped up and enhanced during periods of discomfort and difficulty.
Step 1 of the advice proposed from the DEWS II report is as follows: (6 recommendations)
Recommendation 1: Education regarding the condition, management, treatment, and prognosis.
As previously mentioned, the symptoms of dry eyes vary in intensity and cause. Once patients understand the cause and triggers for their dry eye symptoms, they can start to address the source and possible habits contributing to the condition. Once we understand what the underlying cause may be, we can then assist the patient in personally managing their specific symptoms. For example, if a patient says they have a running, tearing eye, they may not believe the diagnosis of dry eye, without understanding that the reason for their symptom lies in a poor-quality tear film. This means they are lacking a thin fatty layer that is excreted from their lid glands which traps and maintains a stable tear film. The recommended treatment plan for this patient would start with an oil-based lubricant drop or gel to manage the current symptoms, combined with a heat pack to stimulate their own naturally producing oil glands in their lids. This course of action can help to reboot the tear film to do what they are designed for, i.e. to provide a thin fatty layer across the tear film as described.
An initial dry eye assessment gives invaluable information about the underlying cause and thus the management of the condition going forward.
Recommendation 2: Modification of the local environment
There are any number of conditions in patients’ lives that contribute to their dry eye symptoms. We ask patients to consider their workstation at home or in the office, the set-up, hours on tasks, frequency of breaks when on digital devices, excessive air currents around them, blink rate, etc. This can sound like a simplistic approach but is a basic requirement to help promote a comfortable environment. Some practical considerations here can be quickly and easily adopted.
Recommendation 3: Education regarding potential dietary modification (including oral essential fatty acid supplementation)
What we eat affects every part of our body and this includes our tear film. The first thing I ask my patients is how much water they typically consume a day? “Not enough” is generally the answer, so start here if you want to stack the odds in your favour right from the beginning. Much of the food we consume can lead to pro-inflammatory triggers (e.g. some omega 6s) and we are all familiar with the recommendation to take Omega 3. This offsets the effects of the pro-inflammatory triggers mentioned and protects our bodies from a multitude of chronic illnesses and symptoms. There are many Omega 3 supplements on the market but there are 5 elements that will influence how much Omega 3 you actually absorb into your blood, which typically isn´t very much. What effects this absorption is determined by the quality of the Omega 3 supplement itself combined with your health status. The 5 aforementioned elements are as follows:
- The source of the Omega 3, the fish quality, and the potential for contamination, often mercury.
- The manufacturing process and the degree to which the Omega 3 gets denatured during processing
- The storage and packaging of the finished product, best in an individual blister pack format.
- How you take the supplement, with food preferably and with nothing that will denature the Omega.
- And finally, patients with elevated inflammatory symptoms tend to absorb very little Omega 3 and thus fail to reap any real benefits from taking it.
There are many brands of Omega 3 on the market, but we default to Lagad Lacrima as the supplement of choice that addresses the first 3 variables mentioned above at any rate. Lastly, be aware of stimulants and anything that dehydrates you further, e.g. coffee, alcohol, etc. Moderate these if you are going through a difficult dry eye episode.
Recommendation 4: Identification and potential modification/elimination of offending systemic and topical medications.
This is one to discuss with doctor Larry Franks, but certain medications will exacerbate dry eyes. These medications may be more critical to managing your health than any concern about the side effects of dry eye, but perhaps there are alternatives that your doctor will recommend. Some of the medications associated with dry eye symptoms are some antihistamines, anti-depressants, birth control pills, acne medications, blood pressure meds like Beta Blockers, and pain killers.
Remember, Omega 3 is a natural anti-inflammatory and worth including in your daily routine/diet. It should be noted here that there are certain medical conditions that in themselves have a propensity for dry eye as a side effect e.g. arthritis, diabetes.
Recommendation 5: Ocular lubricants of various types
There is a highly confusing array of eye drops and lubricants on the market, so it might be better to categorize them. If you understand what the underlying issue is, then you are informed to select the appropriate drop to treat this cause, e.g. with a tear volume insufficiency use an aqueous-based eye drop. If you have a lipid deficiency, as described in the example above, with a running and tearing eye, there is little benefit to taking an aqueous replenishment eye drop. Our best advice, where possible, would be to select preservative-free eye drops, some manufacturers have removed preservatives at this stage as they have been shown to irritate the eyes.
Eye Drop Categorization
- Aqueous based, usually with sodium hyaluronate as the principal ingredient, the varying concentration determines their effectiveness/lubrication, e.g. Hylo-Tear
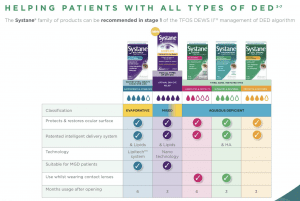
- Lipid-based, commonly propylene glycol e.g. Systane Balance
- Combination aqueous and lipid, e,g, Hylo-dual, Optase spray
- Hypotonic drops, e.g. Hyabak
- Single-ingredient type drops and sprays. Trehalose/Thealoz, Hypochlorous acid/Optase Protect, Perfluorohexyloctane/Evotear
There are also the formulations to consider and which you prefer to use, e.g. drops, gel drops, eye sprays, gel lubricants, etc.
Recommendation 6: Lid hygiene and warm compresses of various types
I cannot emphasize enough that this is an essential part of the daily routine and treatment for anyone suffering from dry eyes. 80% of dry eye patients have shown some degree of blepharitis, usually manifesting in visible scale on the lids. Even when not evident, patients should assume there is a need to clean the lids in the morning, and sometimes in the evenings also, to remove any dead particles or debris that build up overnight or during the day, depending on the living/work environment.
There is a very common lid parasite called Demodex, that lives happily in the eyelids. We have a much better understanding of this parasite now and realise it is very common and increasingly prevalent as we get older, to treat and manage we advise using any of the Tea Tree based lid wipes
There are many lid wipes, foams, and gels on the market which are better than using baby shampoo, as has been recommended for many years. Baby shampoo tends to do more harm than good by removing much of the natural flora and agents needed for a healthy tear film.
In summary, Step 1 has 6 recommendations that are always worth remembering and reverting to.
- Education regarding the condition, its management, treatment, and prognosis.
- Modification of the local environment
- Education regarding potential dietary modification (including oral essential fatty acid supplementation)
- Identification and potential modification/elimination of offending systemic and topical medications.
- Ocular lubricants of various types
- Lid hygiene and warm compresses of various types
There are often simple lifestyle or environmental adjustments that reduce the risk factors. One of the biggest retrograde steps is when people stop their daily routine of lid hygiene, supplement taking, using their heat pack, and instilling their eye drops, when their symptoms appear to have improved. Frustration sets in when the issues resurface. For best results, you need a daily routine during both the good and bad times, only increasing your efforts when needed, but never decreasing or quitting the effort to manage your dry eye.